Genital Herpes: Causes, Symptoms, Treatments, and Light Therapy
In this article, we’ll give an overview of genital herpes and its spread, symptoms, cause, triggers, and treatments, including light therapy.
Questions about genital herpes? Check out this genital herpes FAQs for answers.
What is genital herpes?
Genital herpes is a common and contagious sexually transmitted infection (STI) that may result in recurring outbreaks of pain, itching, rashes, and sores in the genital area and/or anus. Anyone can get genital herpes. In the U.S. it is estimated that close to 1 in 5 people between age 14 and 49 have genital herpes. [1]
There is not a cure for genital herpes, but various treatments like ointments, drugs, and at-home remedies are used to improve quality of life during outbreaks. In this article, we’ll also break down light treatments for genital herpes, and the clinical research being done on phototherapy and herpes simplex virus.
How Does Genital Herpes Spread?
Genital herpes spreads mainly through vaginal, anal, or oral sex, but can also spread by kissing or close contact with someone who has an active infection. Safe sex practices like condoms help prevent genital herpes from spreading. [2,3]
A person who does not have genital herpes can get the virus through contact with the following:
- Another person’s genital herpes sore
- Saliva of a person with oral herpes if they have an oral herpes infection
- Skin near the mouth of a person with an oral herpes infection, or skin in the genital area of a person with a genital herpes infection [1,2,3,4]
It is possible to spread the virus when a person is not showing symptoms or visible sores. Genital herpes does not spread from touching objects or sharing soap. It does not spread from swimming pools, bedding, or toilet seats. [1,2]
What Causes Genital Herpes?
Genital herpes is caused by two kinds of the herpes simplex virus:
- HSV-1, which typically causes oral herpes
- HSV-2, which typically causes genital herpes [1]
The virus enters the body through the mucous membranes in the nose, mouth, and genitals, usually through sexual contact. After the first infection, HSV lies dormant in the body for the rest of a person’s life. Some people experience outbreaks several times a year, but the majority of people never experience signs or symptoms [1]. However, people who don’t experience symptoms can still be contagious to others.
Who Gets Genital Herpes?
Anyone can get genital herpes through contact with sores or people with HSV infections. It is a very common condition, affecting roughly 15% of the United States teen and adult population. [1] Genital herpes spreads most among people who have multiple sexual partners and don’t practice safe sex.
Women are more likely to get genital herpes than are men. The virus is sexually transmitted more easily from men to women than from women to men. [2,3]
Symptoms of Genital Herpes
Genital herpes manifests in outbreaks of painful blisters and sores in the genital area. Sores, blisters, rashes, and itching can occur around the penis, scrotum, vagina, anus, and buttocks. [1,2,3,4]
If symptoms occur, they’re typically the worst during the first outbreak. Symptoms usually appear within two to 20 days after infection, though some people don’t experience an outbreak for years or even decades after contracting the virus. [1] Symptoms can last up to four weeks. [1]
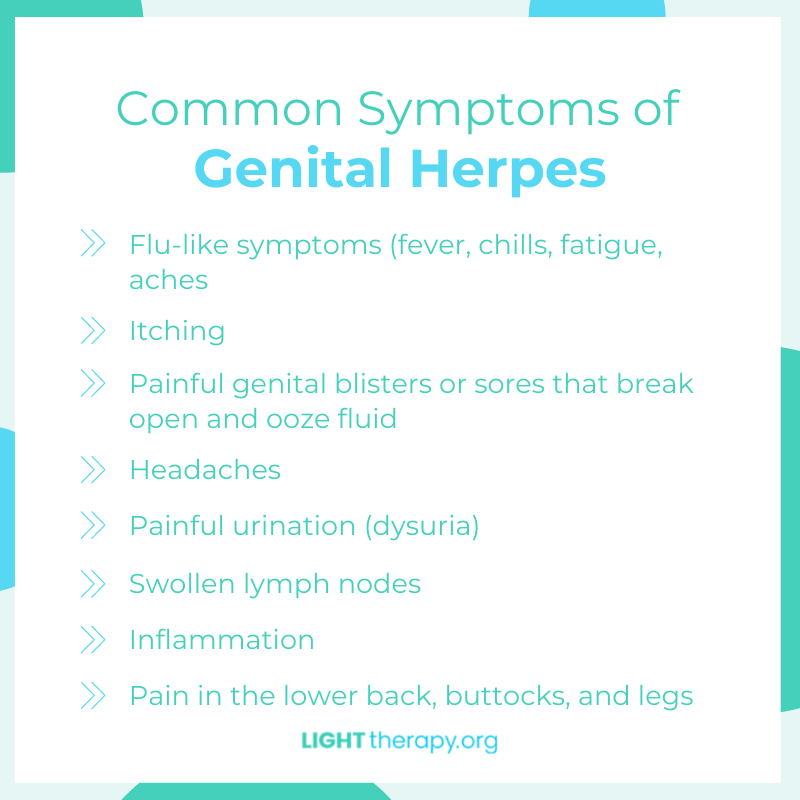
Symptoms include:
- Flu-like symptoms (fever, chills, fatigue, aches)
- Itching
- Painful genital blisters or sores that break open and ooze fluid
- Headaches
- Painful urination (dysuria)
- Swollen lymph nodes
- Inflammation
- Pain in the lower back, buttocks, and legs [1,2,3,4]
Genital Herpes Outbreaks: How long do they last? What triggers an outbreak?
For most people with genital herpes, the symptoms of an outbreak last roughly 2-4 weeks. Some people feel a tingle in the area before a sore develops. During an outbreak, sores may break open and ooze fluid. They usually heal on their own within a month and may develop a scab before they go away. Pain levels associated with blisters and outbreaks vary widely from person to person. For the majority of people with genital herpes symptoms, the outbreaks become less frequent and less severe over time. [3]
Possible Genital Herpes Triggers
Everyone experiences genital herpes and its symptoms differently, and it’s not clear how much lifestyle factors affect the course of the virus. These are among the most commonly reported triggers by people who experience genital herpes outbreaks:
- Sexual intercourse
- Common colds and illnesses
- Sun exposure
- Hormonal changes
- Weakened immune system
- Surgeries/major medical procedures [5]
Diagnosing Genital Herpes & Testing for Genital Herpes
A healthcare provider diagnoses genital herpes by observing active blisters and taking a fluid sample to test for the herpes virus. If a person isn’t having an outbreak, a blood test can check for HSV-2 antibodies, which indicates the virus is present in the body. [1] Some brands also offer at-home testing kits you can buy online and in stores.
Treatments for Genital Herpes
There is no cure for genital herpes or HSV-2. Many people use creams, medications, home remedies, and light therapy to lessen pain and manage outbreaks. Those with less severe outbreaks often choose to let the blisters heal on their own and go away. Light therapy is showing early success limiting pain and reducing viral load in initial peer-reviewed clinical research, summarized below.
At-home Ways to Ease the Pain of a Genital Herpes Outbreak
If you have an active outbreak of genital herpes, the Cleveland Clinic recommends taking the following actions to ease symptoms:
- Keep genitals dry. Moist sores take longer to heal.
- Apply an ice pack. Wrap in a washcloth or apply it over underwear.
- Soak in a warm bath, then dry the area.
- Taking NSAIDs can relieve pain.
- Wear loose-fitting clothing. [1]
Medications for Genital Herpes
Some people take antiviral drugs to improve healing times and relieve pain. Common prescription drugs taken to treat genital herpes symptoms include acyclovir (Zovirax), famciclovir (Famvir), and valacyclovir (Valtrex). These are all taken in pill form, though in severe cases acyclovir may be given intravenously (IV). [6]
Light Treatments for Genital Herpes
Light treatments are used against genital herpes outbreaks to relieve pain and improve healing outcomes. One example of a home-use light therapy device for cold sores is the Luminance RED Genital Treatment Device. Early clinical research has also indicated light treatments may lessen the viral load of HSV-2 present in the body. [7]
How Do Light Treatments Work?
Generally, light treatments work by stimulating your cells to make energy and heal more efficiently. [8] Light treatments have also been shown to reduce inflammation and pain associated with various skin conditions by improving blood flow to damaged tissues. Phototherapy has also been found in numerous clinical trials to increase the body’s antioxidant defenses. [9]
Initial Clinical Research Shows Light Treatments Can Improve Genital Herpes Outbreaks
Numerous clinical studies over the last decade have shown light treatments to be safe and effective for the treatment of various skin conditions. [10]In a pivotal initial study on light and genital herpes, researchers analyzed women with HSV-2 who used phototherapy for three weeks. The study team measured pain levels among the participants before, during, and after the course of treatment, and also used blood tests to analyze the viral load from HSV-2 that was present in the bloodstream. The results show that light treatments can make a major difference for a person experiencing a genital herpes outbreak. [7]
Less Pain from Genital Herpes after Phototherapy
The most notable result from the study was a major reduction in the pain experienced by the patients after using light treatments for genital herpes. Across all participants, the pain was reduced by an average of 82% with phototherapy. [7]
Light Treatments May Reduce Viral Load from HSV-2, Potentially Preventing Outbreaks
In addition to assessing the pain from genital herpes, researchers also conducted blood testing assays to determine the viral load from HSV-2 present in the patients’ bloodstreams. After three weeks of daily phototherapy, the results were “highly significant,” showing a major 60% and 56% reduction in viral load of immunoglobulin G (IgG) and immunoglobulin M (IgM). [7]This result demonstrates that light treatments can not only improve pain and quality of life for people with genital herpes, but also may lessen the overall severity and viral potency of outbreaks. This is a good indication that effective light treatments may prevent future outbreaks or lessen their frequency and severity.
Phototherapy was More Effective than Other Treatments
The study also compared light treatments to topical treatments with honey and ultrasound, a method used around the world to treat HSV-2 and other skin conditions. The researchers showed that light treatments were the most effective method of reducing genital pain and viral load. [7]
Side Effects
The study cited above reported “no significant side effects and herpetic lesions healed faster.” [7] Numerous other reviews of the clinical research on light therapy and skin conditions have found it to be effective for pain relief, healing, and also found light treatments to work “without causing any side effects.” [9,10]
Light therapy doesn’t come with the potential side effects of drugs, but unlike many natural at-home treatments, the science behind light treatments and skin conditions is established in peer-reviewed studies and journals.
Conclusion
Genital herpes is a common, contagious virus that can lead to outbreaks of painful genital blisters. Anyone can get genital herpes by contracting the herpes simplex virus, usually through sexual contact. Some people take medications or let outbreaks heal on their own. Light treatments are also showing potential to improve genital herpes outbreaks in recent clinical research.
As light therapy becomes more widely adopted for the treatment of genital herpes and other skin conditions, it will be important to conduct more clinical trials to standardize treatment parameters.
Sources and References:
[1] Centers for Disease Control. Genital Herpes CDC Fact Sheet.
[2] Cleveland Clinic. Genital Herpes (HSV-2).
[3] Mayo Clinic. Genital Herpes.
[4] Healthline. Genital Herpes.
[5] WebMD. Potential Herpes Triggers.
[6] WebMD. Treatment Options for Managing Genital Herpes.
[7] Waked, Deghidi, and Shalaan. HONEY PHONOPHORESIS VERSUS LOW INTENSITY LASER THERAPY IN FEMALE GENITAL HERPES. IJCRR, Vol. 6, Issue 10. May 2014.
[8] Hamblin M. “Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation” Photochemistry and Photobiology.2018, 94:199-212. 2017 October 31. doi: 10.1111/php.12864
[9] Hamblin M. “Mechanisms and applications of the anti-inflammatory effects of photobiomodulation”. AIMS Biophys. 2017; 4(3): 337–361. doi: 10.3934/biophy.2017.3.337
[10] Avci P, Gupta A, Sadasivam M, Vecchio D, Pam Z, Pam N, Hamblin MR. Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg. 2013 Mar;32(1):41-52. PMID: 24049929; PMCID: PMC4126803.